Unpacking hopes and fears of Karenni Public on Karenni Health Policy: Towards Inclusive Healthcare

Author: Aye Mya Mya Phoo
Advisor: Piyapong Boossabong
Problem Statement
The Karenni state’s healthcare system, involving local healthcare providers, Civil Disobedience Movement (CDM) health providers, and traditional healers, has been crucial in addressing the region’s unique health challenges and needs. The Interim Executive Committee (IEC) ramified an effective healthcare policy focusing on decentralization of service delivery, mobile medical backpack teams, community-based clinics, and the interaction of modern and traditional medicine. The policy aims for Universal Health Coverage (UHC) and will guide the local interim government in delivering effective healthcare services.
Understanding people hopes and fears on policy issues is crucial for improving policy design and implementation. Emotions are underlying forces behind social changes (Boossabong, 2025) and are often ignored in traditional policy development processes. In healthcare, understanding public sentiments is essential for designing policies that respond to societal needs and expectations. As policymakers, it is essential for Karenni health authorities in enabling the emotions of the people to influence policy shaping process, not only policymakers’ visions and goals, in order to transform the policy process to be more inclusive and holistic.
Policy Analysis
The empathetic policy design approach rooted in frameworks like Paterson & Larios’ Empathetic Policy Analysis (2021), argues that emotions shape decision-making always. By recognizing and interpreting human emotions, policy makers can design more effective and empathetic solutions but also consider the emotional impacts of the policies on individuals and communities (Velagaleti, 2024). Healthcare policy development requires in-depth understanding of not only epidemiological data and economic factors, but also the emotional landscape of the public it aims to serve (Hyland-Wood, Gardner, Leask, & Ecker, 2021). The integration of public emotions into healthcare policy is crucial for fostering effective, equitable and socially responsible healthcare systems (Durnová, 2024). Understanding public emotions enables policymakers to craft interventions and strategies that resonate with the lived experiences of individuals and communities, thus increasing the likelihood of positive health outcomes.
Analysing hopeful narratives and fearful narratives of the people
This analysis is done through 3 focus group discussions with 10 participants from Daw Noe Khu Karenni IDP camp. By using “River of Life” and “Dream Clinic” activities, the hopes and fears of people accessing current health services in their area were observed.
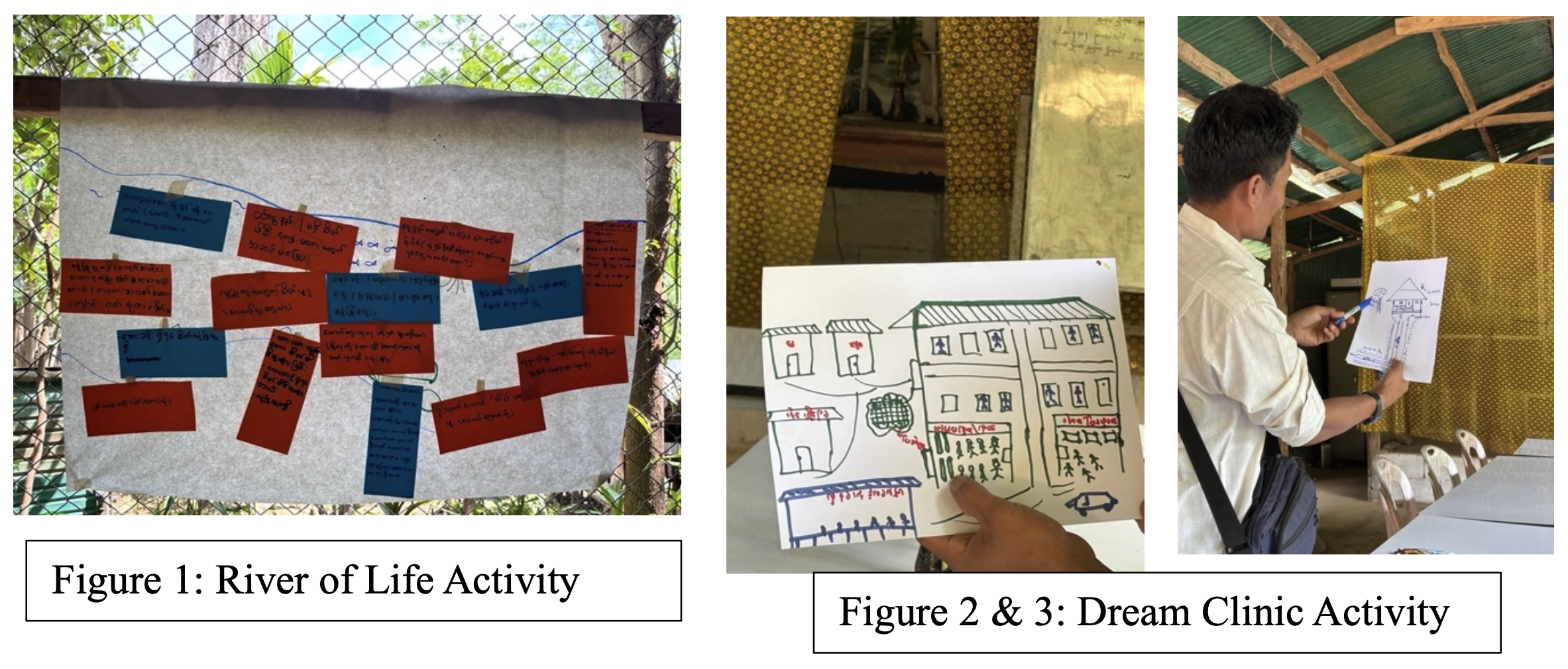
In the River of Life activity, participants shared about their worries and expectations on current healthcare services that they are accessing in the camp. From the discussion and sharing, common fears/ concerns were identified. In the Dream Clinic activity, participants are asked to draw their “dream or ideal” clinic that they want in the next 5 years. This activity primarily revealed their expectations or hopes regarding the healthcare services they want.
One common fear for the people is their security due to frequent visits of SAC’s fighter jets and surveillance drones in their camp area. It was targeted by airstrike in the early hours on 12th July 2023 which destroyed a school and clinic, resulting in serious civilians’ injuries. The camp has since then plagued by frequent jets and drones, causing anxiety and stress among the public. Many participants express concern about accessing clean water, as they use mountain stream water nearby, which becomes murky during rainy season. This leads to skin diseases, especially for young children and elderly seniors. The common hope for the public is undisrupted access to healthcare services. The existing clinic in the camp offer free health treatments, medications, including cross-border referral to Thailand. They hope that they continue to access free healthcare services even after the conflict concluded.
| Shared Hopes (Hopeful narratives) | Shared Fears (Fearful narratives) |
| Undisrupted access to health services
FDG[1]#3 – “I have hypertension and now getting medication from the camp clinic, free of charge. Without the medicine, I could get a stroke. I am thankful for that.” FDG#9 – “I think it’s good that we don’t have to pay for healthcare. We as IDP have no income. We are struggling for putting food on the table. Where do we will get money to pay for healthcare and treatment?” FDG#6 – “I was surprised that all the treatment and medicine were free of charge when I sent my father to the clinic. In Loikaw, there are some costs even visiting the public/government hospitals, let alone private clinics. We could not afford to go even the public hospital because we can’t pay for our transportation to the hospital. I hope we will continue to get free healthcare even after the war end.” |
Fear for security
FDG#1 – “I can’t sleep soundly during the night. The jets come once every two or three days. Every time they come, we run to the bomb shelter with our lives, regardless of day or night.” FDG#4 – “Before we came to this IDP camp, our village’ school was attacked with airstrike. My son who is 14 years old got injured. Since then, he is always scared of jets” FDG#10 – “Now we can differentiate whether it is fighter jet or just surveillance plane by listening to the sound. I was there when we got airstrike back in 2023. I could not stay still for a few months since the attack. I feel anxious and worry about the fighter jets coming back again.” |
| Access to clean water
FDG#1 – “We have to walk for an hour to get clean useable water. I wish we have more clean water sources nearby our home.” FDG#8 – “Now, there are a lot of mosquitos. They came from the water source where we build makeshift dam to accumulate mountain stream water. There are a lot of wrigglers (mosquito larvae) in that water. It would be good if our camp is closed to flowing river or stream.” |
Table 1: Shared Hopes and Fears from FGDs participants
Analysing hopeful narratives and fearful narratives from the Karenni health authorities
The in-depth interviews with three Karenni health authorities revealed concerns about trauma management and mental well-being. They express concerns about providing mental healthcare services while balancing emergency healthcare for live-saving purposes. The Karenni people have suffered physical and mental trauma due to offensive attacks and airstrikes by the SAC. Health authorities are witnessing a growing need for mental health services and express the need for capacity building for health workforce and funding to fill this gap. Two out of three interviewees expressed hopes for health workforce capacity building, with most being medics with experience in emergency healthcare. They hope to train medics into certified health practitioners and nurses, as well as medical doctor and lab technicians. The health authorities believes that healthcare should be accessible to all residents, regardless of ethnicity, religion, citizenship, gender and socio-economic status, and hope to secure long-term sustained funding from both the state government and international aid to continue providing free healthcare to their people. Free healthcare services is an important and necessary part of rehabilitation process in Karenni State, as mentioned by the health authorities.
| Shared Hopes (Hopeful narratives) | Shared Fears (Fearful narratives) |
| Health Workforce Capacity Building
HA#1 – “We sent five nurses to Mae Sot to attend 3 years nurse training. I am hopeful that they will come back and work with us to train the rest of the medics.” HA#2 – “We have plan to co train our medics with CDM doctors and nurses. They could help us build our health workforce to a higher level.”
|
Mental Health Services
HA[2]#1- “I can see there are many cases of hypertension in the IDP camps. Stress is the main root cause of this. They stress about their safety; they stress about food for their families. Sometimes, there were even suicide cases.” HA#2 – “It is true that we have a mental health medic in Daw Noe Khu and it is very helpful to the public. They can go and talk with her when they feel stressed. We need more medics who can also offer counselling service.” HA#3 – “Sometimes we have to prioritize emergency care over mental health care. But we should acknowledge that metal health is equally important as physical health.” |
| Free Healthcare Services
HA#1 – “I think we should continue to provide free healthcare services to our people even after war. It is a part of rehabilitation process. We can think about private healthcare systems or health insurance later after we strengthen our own healthcare system.” HA#2 – “It is necessary for people to get access to free healthcare even after the revolution has won. Our people lost their homes and farmlands. How can they pay if we charge for healthcare?” |
Table 2: Shared Hopes and Concerns from in-depth interviews with health authorities
Conclusion and Recommendations
Based on the analysis of hopeful narratives and fearful narratives from both the public and health authorities, policy recommendations that address to their hopes and fears are crafted. One common hope shared by both the people and health authorities is “Free Healthcare services” and the same recommendation is made to address this shared hope.
| Hopes (Hopeful narratives) | Fears (Fearful narratives) | Required policies |
| People | People | |
| Undisrupted access to health services | Fear for Security | 1) Sustained free essential healthcare for all the people in Karenni State by securing long-term funding from the state government and international aid.
2) Fund reinforced bomb shelters in high-risk areas (Schools/clinics). |
| Access to Clean Water | 3) Train community members in water purification technique under WASH program (using sand, charcoal). | |
| Health Authorities | Health Authorities | |
| Health Workforce Capacity Building | Mental Health Services | 4) Provide mental health training to existing medics under capacity building program.
5) Assign mental health counselor position in existing mobile backpack team structure (2 medics, 1 trained birth attendant, 1 in-charge, 1 Lab medic). |
| Free Essential Health Services | 1) Sustained free essential healthcare for all the people in Karenni State by securing long-term funding from the state government and international aid. |
Table 3: Shared Hopes and Concerns from in-depth interviews with health authorities
Policy Recommendations and Stakeholders
(1) Sustained free essential healthcare for all the people in Karenni State by securing long-term funding from the state government and international aid.
Stakeholders: Karenni interim government, health authorities, CDM doctors and nurse association, international funding agencies
The shared understanding between the health authorities and the people is that access to free essential/primary healthcare is vital part of the rehabilitation process. As the interim governing mechanism of Karenni State is gaining control over the territory, it is important that public services such as education and health care are guaranteed to their public regardless of their socio-economic status. The provision of essential healthcare services without financial burden on the public can be also seen as trust building process as well as asserting sovereignty.
(2) Fund reinforced bomb shelters in high-risk areas (Schools/clinics).
Stakeholders: IDP camp committee, Karenni interim government, school committee, teachers, medical professionals, public
Due to the target attacks on schools and clinics by the SAC fighter jets, it has become essential that schools and clinics have reinforced bomb shelters. The NUG together with ethnic governing bodies are building up bomb shelters and using them as schools and clinics so that the risks can be mitigated for the vulnerable populations in the camp.
(3) Train community members in water purification technique under WASH program (using sand, charcoal).
Stakeholders: IDP camp committee, Karenni Health Department, Karenni Community Development Groups, public
Setting up low-cost water purification system in the camp community can increase access to clean and usable water. Prevalent skin diseases among the people are mostly caused by the unfiltered water source. Using locally sourced material such as bamboos, charcoals, river stones and sand, the community can be trained to set up water purification systems in the camp to help with the clean water supply. It requires minimal budget, yet sustainable because the materials can be sourced locally and without additional costs from nearby forest.
(4) Provide mental health training to existing medics under capacity building program.
Stakeholders: Karenni Health Department, Health authorities, Medics, existing funders, CDM mental health professionals
As the conflicts persist in the country, the mental health challenges become severe for the people including service providers. Currently, lifesaving trainings and first aid training are being organized as priorities, yet it is also important to acknowledge that mental health is equally important as physical health for the people. Providing mental health training to existing medics with the support from CDM mental health professionals can improve the health services the Karenni Health Department is providing to the people.
(5) Assign a mental health counselor position in existing mobile backpack team structure (2 medics, 1 trained birth attendant, 1 in-charge, 1 Lab medic).
Stakeholders: Karenni Health Department, Health authorities, Medics, existing funders
From the FGDs and in-depth interviews, there were serious concerns for mental health situation of the people in conflict setting. Most of the FDGs participants went through traumatic experience during the bombing attacks by SAC or battles. Forcibly displaced by their homes due to the attacks, they have faced with livelihood challenges in the IDP camps, which further push them to become distress. Some lost their homes and loved ones on their journey for survival and must deal with the loss without proper support systems. There have been some suicide cases and suicide attempt cases in the IDP camps due to the hardships and stress they face day to day basis. Support for mental health become a lifesaving health service in this scenario.
The current Karenni healthcare system is operated mainly by mobile medical backpack teams and community-based clinics. With their medicine filled backpacks and a team of medic on the move, they can provide essential healthcare services to the people who are the most in need. Mental health service can be delivered through the backpack teams when one of the medics can be trained and assigned as a community counsellor. The community counsellor will be equipped with basic mental health knowledge and counselling skills so that the medic can provide counselling to the people when the team goes outreach trips.
Limitations of the Policy Research
As the research was conducted on small scale with a selected small number of participants, it might not truly reflect the magnitude of hopes and fears of the people when accessing healthcare services. The research can be further developed with additional observation on how public react to the proposed policy recommendations in the research, using “Emotions based Sentiment Assessment Tool”. This method can clarify if these policy recommendations respond to their hopes and fears on the access to healthcare services.
References
[1] Boossabong, P. (2025). Empathetic policy design. https://doi.org/10.1007/978-3-031-75002-1
[2] Durnová, A. (2024). Psychosocial well-being, policies, and the emotional boundaries of home. Critical Policy Studies, 1. https://doi.org/10.1080/19460171.2024.2306237 .
[3] Hyland, B., Gardner, J., Leask, J., & Ecker, U. K. H. (2021). Toward effective government communication strategies in the era of COVID-19. Humanities and Social Sciences Communications, 8(1). https://doi.org/10.1057/s41599-020-00701-w
[4] Paterson, Stephanie, and Lindsay Larios. 2021. Emotional Problems: Policy- Making and Empathy Through the Lens of Transnational Motherhood. Crit- ical Policy Studies 15 (3): 273–291. https://doi.org/10.1080/19460171. 2020.1752760.
[5] Velagaleti, S. (2024). Empathetic Algorithms: The Role of AI in Understanding and Enhancing Human Emotional Intelligence. Journal of Electrical Systems, 20(3s), 2051–2060. https://doi.org/10.52783/jes.1806
Note:
[1] FDG# – each participant in focus group discussion is given a number.
[2] HA – Health Authority
Download full article: Click
